Laboratory Testing Services Manual - Specimen Collection and Submission Form Guidance
Testing at the DSHS Laboratory
Each year, the DSHS Austin Public Health Laboratory receives approximately 1,500,000 clinical specimens, food and water samples, environmental samples, biological and chemical compounds, and biological agents for testing.
- The Newborn Screening Program receives approximately 780,000 newborn screening specimens each year.
- Newborns’ blood spots are tested for 55+ metabolic and genetic disorders.
- The Microbiology Laboratory receives approximately 250,000 specimens each year.
- The Rabies Laboratory receives 6,000 to 9,000 rabies specimens each year.
- The Laboratory also collaborates with the Texas Commission on Environmental Quality to test water from over 7,000 public water systems across Texas for coliforms.
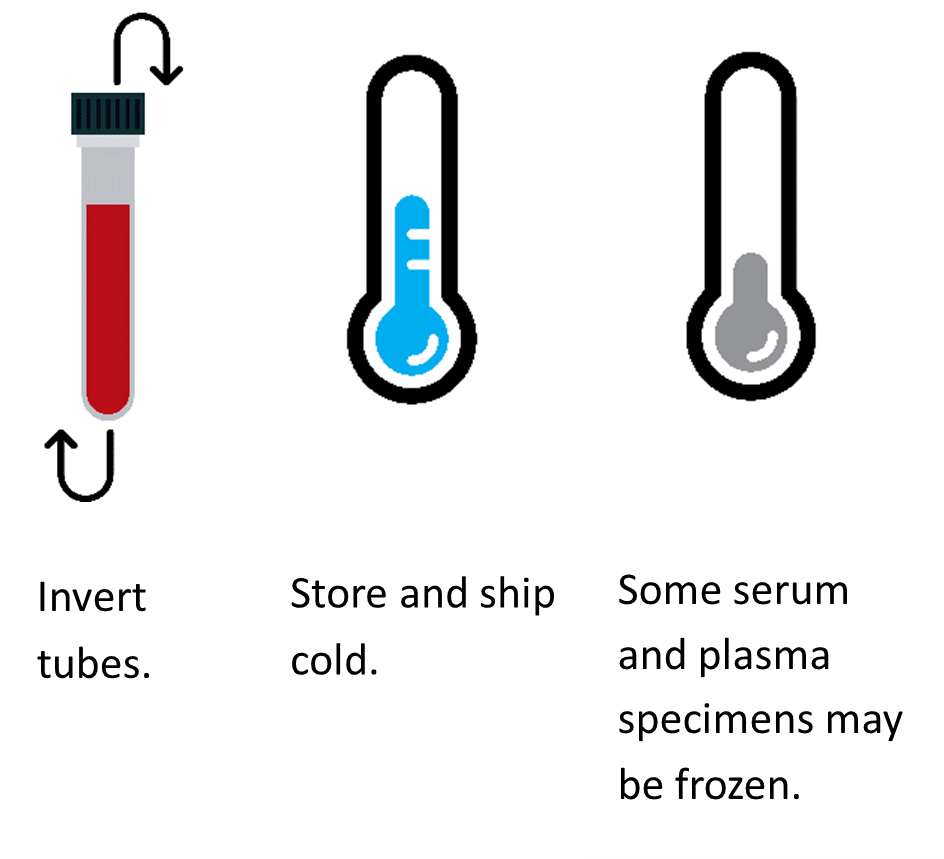
This guide was developed to help submitters with the DSHS Laboratory specimen submission process and to avoid the most frequent causes of specimen rejection.
The guide is provided for all submitters to the DSHS Laboratory. These include, but are not limited to physicians, licensed commercial laboratories, health care facilities, local and regional health departments, veterinarians, animal control officers, law enforcement officers, and members of the public (for water testing and rabies testing only).

















 ACCEPTABLE
ACCEPTABLE NOT ACCEPTABLE
NOT ACCEPTABLE